Bringing prescription price transparency to the point-of-care seems like a simple concept. But myths about Real-Time Prescription Benefit (RTPB) technology are making it more difficult to understand what is real when it comes to the solutions available in the market. RxRevu has successfully deployed RTPB at over 2,000 hospitals and health systems, and we think it is important that teams know the truth about RTPB. Below are the most common myths we hear when speaking with healthcare leaders from across the industry.
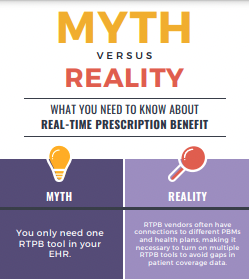
- The most common myth we hear is that health systems only need one RTPB vendor turned on within their EHR. However, since each RTPB vendor has connections to different PBMs – and therefore has access to different subsets of patient data – it is essential that health systems connect to more than one vendor to avoid gaps in patient coverage. RxRevu works with many health systems that have upwards of two or three RTPB connections. And while RxRevu has coverage data on over 150 million patients, we do not have data on everyone (nobody does). Health systems should think strategically about their patient population, and should not assume their work is complete when one prescription price transparency tool is turned on. Instead, teams can avoid provider frustrations by enabling multiple connections to fill data gaps.
- There are a number of RTPB vendors who claim to have ‘all-payer’ solutions. While we know this is simply impossible – since not every PBM has turned on connectivity for RTPB – these vendors typically use aggregated or historic data to estimate medication costs. This creates the illusion of an ‘all-payer’ solution, but in reality, these tools often do not bring accurate pricing information to the point-of-care. This leads to a negative provider and patient experience, since unreliable data may give inaccurate price estimates – causing patients to pay more for their medications than expected.
- Many IT and physician leaders worry that implementing a RTPB tool will disrupt their project queue, require hours of training, or create friction in the EHR workflow. In all of these cases, the opposite is true. RxRevu has developed a streamlined process for implementing RTPB within a health system’s EHR, typically needing only 8-10 hours of IT time to configure and set up medication display rules. Further, EHR vendors can often provide short training modules – grouped with regularly scheduled training sessions – to teach providers about how to search for prescription cost and coverage information. RxRevu can supplement these training sessions with materials about how to use RTPB, but what we’ve found, is that providers actually leverage the tool without any training at all. Finally, using a RTPB solution does not increase friction in the EHR. When submitting a medication order, providers can either request a cost estimate, or they will be prompted to confirm the order if there are lower-cost, covered alternatives available. RxRevu understands that complicated processes and unnecessary data will hinder adoption. That is why we’ve seamlessly integrated our RTPB solution to reduce clicks and create a better overall provider experience.
- Lastly, our team has heard from health system leaders who do not trust RTPB tools because they think the coverage and cost data displayed is not accurate. While some vendors utilize outdated flat files or historic information, RxRevu delivers real-time data directly from our PBM partners to health system EHRs. We pride ourselves on our data accuracy, and because we do not rely on aggregation or estimation, we are able to bring patient-specific pricing to the point-of-care, more often than any other vendor.
Having price transparency information at the point-of-care can improve both patient and provider experiences, while helping reduce unnecessary workflow burden and medication spend. But being able to trust your data – and your RTPB vendor – is of the utmost importance. RxRevu is committed to creating the most reliable and accurate decision-support tool in the market. Through this post, we hope to clarify some of the common myths and misconceptions about RTPB.
To share this information with your team, feel free to download our mythbusters infographic. And if you would like to learn more about RxRevu’s Real-Time Prescription Benefit solution, please reach out today.